The Evolving Landscape of Serotonin Receptors and Mental Health Treatment
Explore blog posts directly from the team at David Salvage, MD in Brooklyn, NY.
Get in Touch

Explore blog posts directly from the team at David Salvage, MD in Brooklyn, NY.
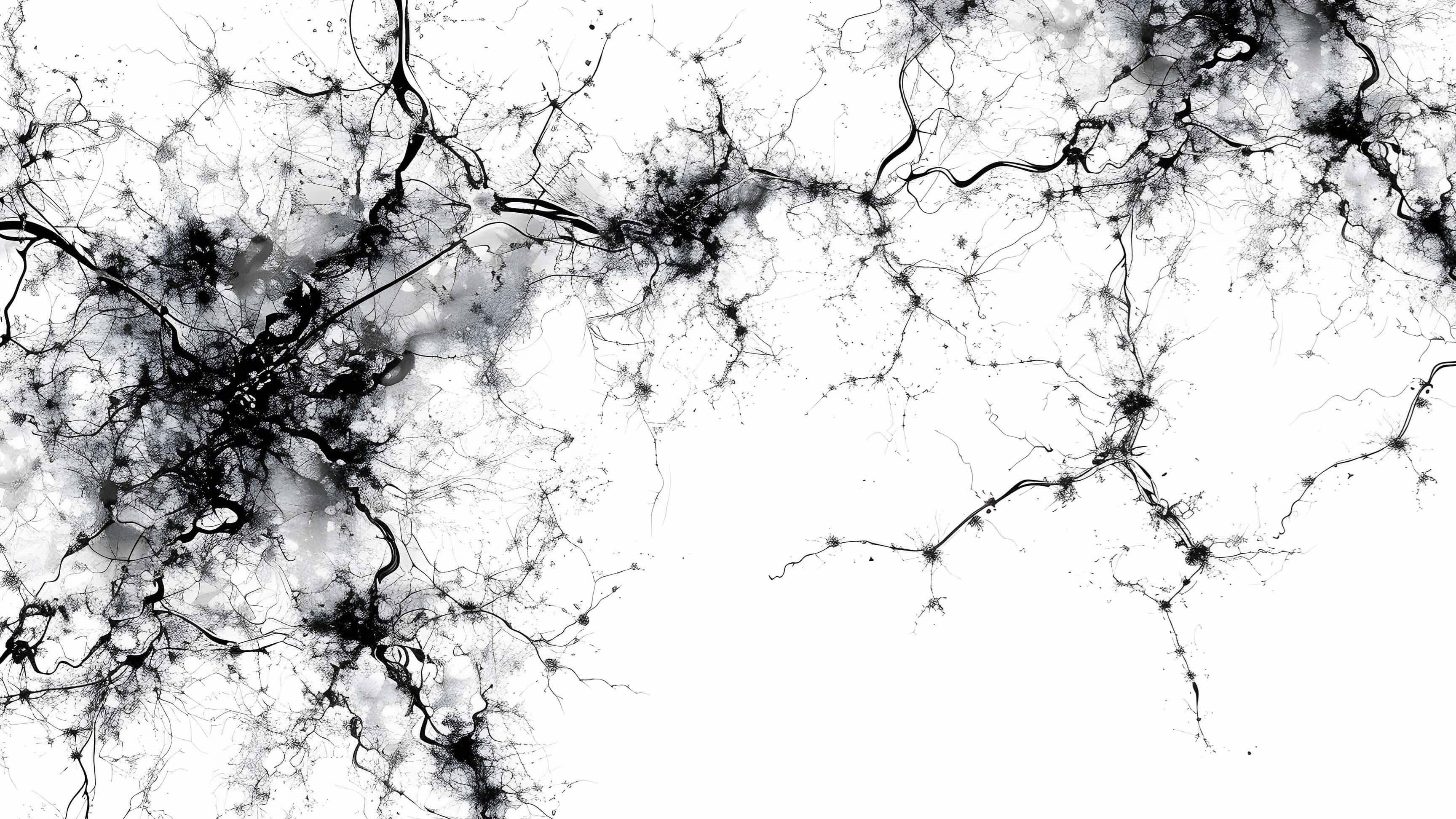
Get in TouchIn 1990, our understanding of the brain's serotonergic system was relatively simple. At that time, scientists had identified just two types of serotonin receptors. Fast forward thirty-five years, and the picture has changed dramatically. We now know of over one hundred serotonin receptor subtypes, each with a myriad of subunits and complex interactions. This explosion in knowledge has transformed the way we understand—and treat—mood disorders like depression and anxiety.
With these discoveries came both promise and complexity. On the one hand, more receptor targets have meant the development of more sophisticated medications. Today’s pharmacologic toolbox is rich with options designed to target specific aspects of serotonin signaling. On the other hand, this abundance has also made the task of choosing the right medication more intricate than ever.
The result is a paradox: treating depression and anxiety has become simultaneously more hopeful and more challenging.
This is where the expertise of skilled psychiatrists becomes critical. With dozens of antidepressants and anxiolytics now available—each with distinct receptor targets, side effect profiles, and efficacy patterns—psychiatrists must navigate a complex web of potential treatment paths. No longer is it a matter of simply selecting a standard SSRI and waiting for results. Instead, effective psychopharmacologic management often involves a nuanced understanding of receptor subtypes, genetic predispositions, co-occurring conditions, and patient response patterns.
In essence, psychiatry is no longer just an art—it is increasingly a science grounded in neurobiology and personalized medicine. The ability to guide patients through the ever-evolving algorithms of treatment requires not only medical knowledge but also patience, adaptability, and a deep commitment to the therapeutic relationship.
For patients, this means there is more hope than ever before. The expanding range of treatment options allows for highly tailored approaches—ones that can address treatment-resistant cases or minimize intolerable side effects. But it also underscores the importance of working closely with a knowledgeable provider who can interpret this complexity and turn it into a clear path forward.
The brain, it seems, is even more intricate than we once believed—but so is our ability to heal it.
